As we get older, our muscles and bones gradually weaken, a progression that can lead to falls, fractures, and a devastating cycle of hospitalization and physical decline. But not everyone experiences this decline at the same rate—social and economic conditions over a lifetime can profoundly shape how the body ages, influencing access to nutrition, physical activity, and preventive health care. New research co-published by Gustavo Duque, the Dr. Joseph Kaufmann Chair in Geriatric Medicine and professor in McGill’s Department of Medicine, suggests that a patient’s position on the socioeconomic ladder may play a significant role in how quickly that deterioration occurs—and that the disadvantage begins well before a patient ever reaches a hospital.
The study examines the relationship between socioeconomic status (SES) and bone, muscle, and physical function in 300 community-dwelling adults aged 50 and older in the metropolitan region of Melbourne, Australia. Researchers measured five indicators of SES—education, income, employment, health care card ownership, and area-level disadvantage—against outcomes including bone mineral density, muscle mass, grip strength, gait speed, and leg power.
Notably, the researchers found that participants who completed post-secondary education had significantly higher bone mineral density, greater muscle mass, stronger handgrip strength, faster walking speed, and greater leg power than those with less education. Higher income and possessing a private health care card—as opposed to a government health card—were similarly associated with better outcomes across most measures.
Duque said in an interview with The Tribune that the findings confirmed what the research team had long suspected.
“People with lower levels of income and lower levels of education […] were the ones who showed the worst situation in terms of muscle and bone,” Duque said.
One unexpected finding is that employed participants showed different patterns of deterioration, regardless of salary. Duque attributed this to the physical demands of their work, noting that those still employed tended to be active throughout the day. For those who were retired or unemployed and in the lowest socioeconomic brackets, however, the outcomes were markedly worse.
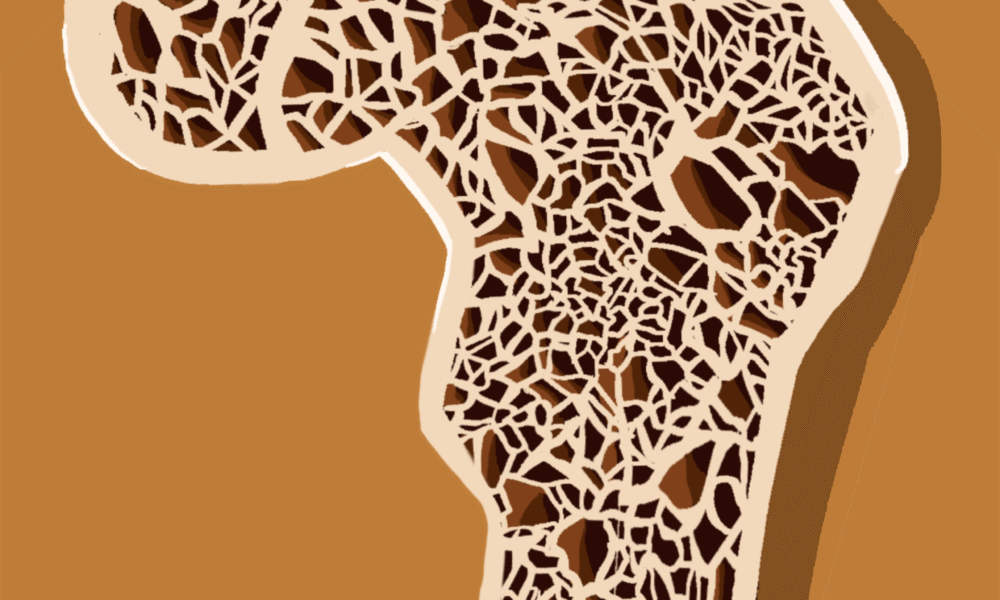
Osteoporosis, a condition characterized by low bone mineral density, which ultimately raises the risk of fractures, affects approximately 18 per cent of older adults globally. Sarcopenia, the progressive age-related loss of muscle mass and physical function, affects between 10 and 27 per cent of individuals over 60. Although a growing body of work links SES to musculoskeletal health, evidence on how social gradients operate in specific musculoskeletal conditions such as sarcopenia and osteoporosis remains limited. Prior studies have typically relied on secondary analyses of existing datasets rather than directly investigating the relationship.
Since the study is cross-sectional, it captures a snapshot of health outcomes at a given point in time and cannot determine whether interventions would prevent or reverse the disparities observed. Duque acknowledged this limitation, which is why his future research aims to explore the longitudinal impacts of socioeconomic status on bone and muscle decline.
The study also raises questions about health literacy—the ability to access, understand, and apply health information—as a potential mechanism linking a lower SES to worse musculoskeletal outcomes. Both osteoporosis and sarcopenia require patients to adopt and maintain lifestyle changes such as increased physical activity and dietary adjustments. However, lower education and income are strongly correlated with lower levels of health literacy, meaning that socially disadvantaged groups may be less likely to receive, understand, or act on prevention and treatment advice. Consequently, the same communities that enter older age with weaker bones and muscles are also the least equipped to access the information and resources needed to slow that decline, further entrenching existing disparities.
Duque stressed that prevention does not need to be expensive or complicated.
“It does not demand a lot of resources. A good physical activity can be done in a park or in a mountain,” Duque said. “There are some dietary recommendations, […] there are good sources of calcium that do not necessarily have to be very expensive.”
But he also emphasized that individual behaviour change alone is not enough, and that policy-level action is essential.
“We need a policy [….]The problem is that some of these policies are not necessarily applied, developed, or funded,” he said.Duque’s team is now launching a Quebec-based screening project in collaboration with the World Health Organization to identify musculoskeletal decline early in older adults across the province. Musculoskeletal data cannot close the socioeconomic gap in bone and muscle health alone, but knowing where that gap starts is the first step toward designing interventions that effectively address it.