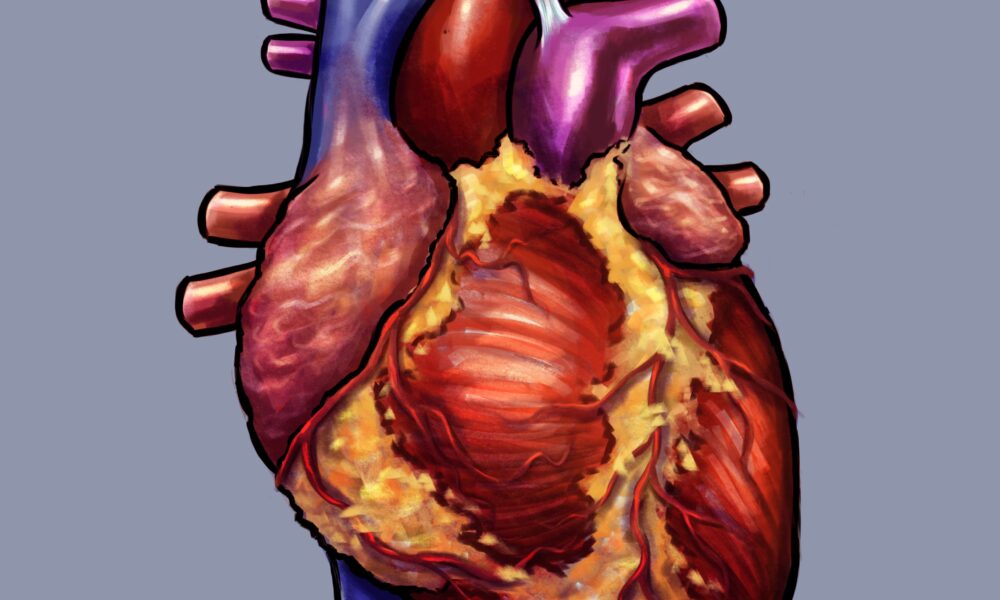
Human heart transplants have revolutionized treatments for terminally ill cardiac patients for the last 117 years, but a lack of donors has meant that every year, thousands are left with no other option than to wait on a seemingly endless waitlist. To combat this shortage, researchers are looking into other experimental approaches, including bioprinting, the use of engineered organs, and the transplantation of genetically-engineered pig hearts into humans.
Xenotransplantation—transplants that use organs from a different species—has been employed in a number of procedures, ranging from small skin grafts to entire kidney transplants. While the field has been around since the 19th century, it only recently started showing signs of success through the use of genetic engineering. On Jan. 7, 2022, years of research culminated in the first successful heart transplant from a pig to a human patient.
A cardiac patient at the University of Maryland Medical Center, David Bennett Sr. was ineligible for a traditional heart transplant due to the severity of his arrhythmia. His last resort for treatment was to undergo an experimental pig heart xenotransplant. Post-surgery, the 57-year-old patient remains stable, marking this procedure a success and a milestone in transplant history.
What distinguishes this successful transplant from previous attempts is that scientists genetically engineered the donor animal organ prior to surgery—a procedure vital in preventing the patient’s antibodies from rejecting the foreign material. Pig cells produce a sugar called alpha-gal that causes a fatal immunological reaction when transplanted into humans. To ensure a fully functional transplant, scientists must modify the donor genes to eliminate this sugar. On top of the removal of alpha-gal from the pig heart, six human genes were inserted into the pig heart to decrease the risk of rejection, while the three pig genes that caused an immunological reaction were removed. The researchers also removed an additional gene to prevent any excessive growth of the pig heart.
J. Matt Kinsella is an associate professor in the Department of Bioengineering at McGill whose research focusses on tissue engineering and bioprinting. In an interview with The McGill Tribune, he highlighted the risks of organ transplants using gene-edited tissues.
“A few of the challenges are getting the genes to the site where you want the function to occur,” Kinsella said. “If you try and just deliver a gene systemically to a person, it’s not a targeted system that would go directly to your cardiac tissue, it can go anywhere. You can knock out gene tissues that shouldn’t have that gene knocked out.”
While the risk of using gene-edited animal organs offers hope for those on transplant waitlists, there are still many ethical debates surrounding the procedure. Many view xenotransplants as a form of unnecessary animal cruelty, while others think its potential to save many human lives outweigh these concerns.
“I think that might be what is missing right now, the public opinion on a lot of this work,” Kinsella said. “On the scientific side, we find it very fascinating that we can do this, but it came out pretty quick and I don’t know that there’s been much consultation [with] the public.”
In fact, the Food and Drug Administration only approved the procedure because it was the patient’s only remaining option.
As biomedical and bioengineering fields develop, scientists can avoid using living organisms as organ donors by looking toward tissue engineering and bioprinting in transplants. However, these complex fields are not advanced enough to perform procedures at the organ level yet. Such transplants are not suitable for every patient, either, as some people are more susceptible to allergies or have adverse reactions to biomaterials.
“To complete an entire anatomically correct, functioning heart is something we are still very far away from,” Kinsella said.
The first successful heart xenotransplant, although controversial, is a critical turning point in the evolution of organ transplants and a valuable learning opportunity for many researchers to better understand the influence of genetics on the field of biomedicine.








Transgenics and transhumanism are sins against nature and God. These unethical practices are forbidden by God. God forbid the mingling of seed or genetic modification of a species with a different kind of species. ( Leviticus 19:19) God intended that species of the same kind only reproduce with each other. ( Genesis 1:24-25) Splicing and genetically modifying DNA from one species to another is what would cause the wrath of God to be poured out without measure.
The Blog is a good read, I got to know valuable information about the topic. I will definitely reccommend this to my peers and family members. I am also interested in this topic and found some wesite regarding the same. Check out this site to know more about the topic
https://www.manipalhospitals.com/blog/heart-transplant-procedure-risks-and-recovery/