Data science and machine learning, a branch of artificial intelligence (AI), may soon be making their way into operating rooms as integral parts of the surgical toolkit. The Feindel Brain and Mind Lecture Series tackled this cutting-edge development at its Nov. 2 event hosted at The Montreal Neurological Institute-Hospital. Pierre Jannin, a L’Institut national de la santé et de la recherche médicale (INSERM) research director working at the University of Rennes medical school, discussed AI in relation to deep brain stimulation (DBS), something he has worked on extensively.
DBS involves implanting an electrode in the brain that continuously provides high-frequency electrical stimulation. It can help patients with neurological movement disorders, such as Parkinson’s disease, and treat debilitating symptoms like tremors and movement issues that cannot be alleviated using medication.
During a typical DBS procedure, the surgeon is assisted by a team of experts, including nurses, an anesthesiologist, and an electrophysiologist, and devices like an anesthesia machine and an EKG machine. Despite all of these external resources, the surgeon must monitor essential information such as the position of the electrode and the patient’s vital signs all on their own.
“The visualization and interaction approaches are very important […] for surgeons who are dealing with images and information. We have to help them in digesting all this information,” Jannin said.
Jannin explained that surgical data science can optimize the surgical workflow by helping surgeons use all of the tools at their disposal more efficiently. The ultimate goal of using data science before, during, and after the procedure is to facilitate the surgeon’s decision-making and to optimize the clinical outcome of the patient.
“To summarize the idea of surgical data science, you have three main flows. First, you learn from patient data. Second, you instantiate this new information to generate new knowledge, and third, [the application of surgical data science] is a continuous process,” Jannin said.
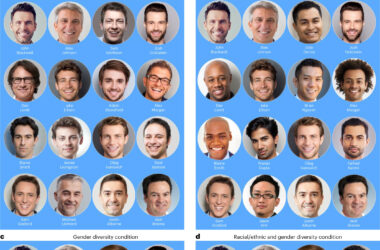
With the help of his team, Jannin has established a machine learning model to extract information about a patient’s age, gender, and potential cognitive deficits from their medical records. This information is then added to a data repository and analyzed to generate models for treatment that can be applied to a wide range of patient cases.
The team thus develops generic knowledge-based templates that can be used to create patient-specific models. Jannin noted that one possible application of this model is predicting the clinical outcome of DBS in a patient.
“We aim to improve the quality of surgery, of the healthcare, and […] of course, it is about the patient outcome, the clinical outcome, but […] also […] the working conditions of the professional,” Jannin said.
Jannin mentioned a few obstacles that surgical data science could help physicians overcome. For instance, surgical data science can increase the accuracy of brain region targeting in the preoperative stage, which is crucial because the electrode’s placement corresponds to the brain area that will be stimulated. When it comes to Parkinson’s, DBS targets the subthalamic nucleus (STN), a small structure important for motor function.
Typically, during surgery, the electrophysiologist, an expert in the electrical phenomena of the nervous system, listens to the neuronal signals of the STN neurons to locate the STN.
“We recently developed a deep learning based approach that can recognize the STN’s auditory signal in a more objective way and [its accuracy] is roughly the order of uncertainty of the electrophysiologist,” Jannin explained.
Once an operation is done, researchers feed different clinical scores for factors like motor skills and quality of life into the software to compare patients’ results and to verify DBS’s efficacy.
“It’s important to demonstrate how this kind of decision support system will bring added value,” Jannin said. “So it’s great to put AI tech everywhere […] but it’s also important to discuss with the clinicians themselves and see if they will trust this kind of technology and where exactly it could be useful.”