Despite the meteoric rise of plant-based milk’s popularity over the past few years, cow’s milk continues to dominate the global milk market. It is an excellent source of vital minerals, vitamins, and proteins, and is often recommended for young children—that is, assuming they are not allergic. Even with all of its essential nutrients, cow’s milk allergy remains the most common food allergy among children. Furthermore, this allergy is typically cross-reactive with goat and sheep milk due to similarities in the milks’ proteins, although this is not always the case.
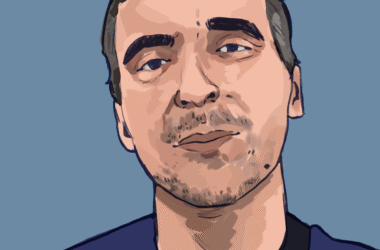
In a recent report published in Allergy, Asthma, & Clinical Immunology, Dr. Michael Aw, a resident physician in Internal Medicine at McGill University, detailed the unusual case of a 27-year-old Mediterranean man who developed an allergy to goat and sheep milk, but not to cow’s milk. Despite having no issues with goat and sheep milk for most of his life, the patient later experienced anaphylactic reactions after having goat- and sheep-milk-based cheeses. Doctors later confirmed his allergies with skin prick tests, and it was during these tests that they discovered the lack of cow’s milk sensitization.
In an interview with The Tribune, Aw explained how this co-occurrence of cow, goat, and sheep milk allergies typically works.
“Goat milk and sheep milk allergies are not a very rare thing. It’s a relatively common allergy, but almost always it’s because people were pre-sensitized to milk allergy,” Aw said. “We were often exposed to milk protein because of our diets, and definitely in a Western society. Milk, cheese, and all sorts of even pre-made or dried products contain cow’s milk. And often people who get allergic to one type of food can get sensitized to a bunch of foods within the same family, because the protein structure that you’re allergic to is very similar between the different animals or the different species.”
Aw further explained how the initial sensitization to cow’s milk occurs, pointing in particular to the milk’s immunogenic proteins, which can induce an immune response and cause an allergic reaction. In the case report, the patient appeared to be sensitive only to immunogenic proteins in goat and sheep milk, not to those in cow milk.
“The main two classes [of milk proteins] are casein and whey,” Aw said.“Whey protein, which is a collection of different proteins, loses some of its allergenic properties when you heat it up because you denature the protein. The protein and its structure become deformed, and it’s no longer as immunogenic, versus casein, which can maintain [its structure]. With milk allergy, some people are sensitized to particular epitopes, or parts of the protein, of the casein within goat milk that is just different enough to cow’s milk, that they don’t react [to cow’s milk].”
When conducting a literature search on isolated goat and sheep milk allergies, Aw found that the vast majority of studies corroborated the hypothesis of sensitivities to particular casein epitopes. They noted that these kinds of goat and sheep milk products are typically consumed after being made into cheeses, which is a process that denatures the whey and leaves only the immunogenic casein behind.
Another factor that made this case slightly unusual was that the patient developed the allergy in adulthood. While it is not uncommon to develop allergies later in life, children are more susceptible to them.
“A lot of things in immunology are unknown, but proposed hypotheses or mechanisms are, just how a baby’s developing, its immune system is developing, and it’s not very well educated,” Aw said. “So an immune system that’s not well educated isn’t very specific or well-adjusted [….] It’s getting exposed to all of these different allergens and antigens, and it doesn’t really know how to differentiate between good and bad. And that’s why children often react to foods which they then outgrow, because as their immune system matures, they are better able to tolerate it.”
As infants, our immune systems are hyper-aware of differences in the nutrients we ingest because these substances are relatively new to us; this potentially contributes to our tendency to develop allergies during those years.
“There’s a distinction between cow’s milk and human’s milk, where it’s just different enough that your body is used to human’s milk, and the extra proteins that you don’t see in human’s milk that you see in cow’s milk kind of freaks out the immune system [….] If you get exposed to it enough times and nothing bad happens, sometimes the immune system forgets and develops what we call a tolerogenic profile, amongst other factors that can cause you to ‘outgrow it,’” Aw explained.
However, as mentioned, for our patient of interest, this was no childhood allergy.
“Allergies can occur, unfortunately, at any time in life, and it just takes a bit of bad luck to just have food at the wrong time, the wrong place, with the wrong co-factors that caused you to get sick or to cause you to develop an allergy,” Aw noted.
Aw also pointed to the diversity of circumstances under which adult allergies can develop.
“Sometimes it’s people who have never seen a food or an allergen for many years, and then when they get re-exposed, the immune system overreacts,” he said. “But sometimes, it’s people that work with the same chemical, the same food their whole life, and then just one day, the immune system decides, you know, ‘Enough is enough, and we’re going to be allergic.’ To really see why it happens is very nuanced and a poorly understood mechanism. But yeah, it just happens.”
While this case was certainly interesting, Aw noted that randomized control trials and further meta-analyses of said trials would need to take place in order to make any general statements about differences in milk allergies overall.
“With a case report, people like to get excited [and think], ‘Oh, is this going to be the next big thing?’ I always like to highlight the fact […] that a case report is the lowest level of evidence in any medical reporting [….] We’re just saying, ‘This is what we observe.’ It’s very hard to draw conclusions from this. I think the big takeaway from this paper is to be aware that it exists.”
Aw clarified that the purpose of a case report like this, at least in his view, is to provide clinicians with an unusual case of milk protein sensitivities they can keep in the back of their mind. This can be useful if they witness something similarly odd in their own practice.
“Just because someone can tolerate cow’s milk may not necessarily mean they can tolerate goat milk or sheep milk. Do we recommend that you target a test specifically for that? No, not necessarily, but […] just know that it’s possible that they may not tolerate goat and sheep milk.”
Immunology is one of the most misunderstood fields in medicine, by both the general public and the medical community. Myths circulate long and widely enough that they become difficult to eradicate, so much so that they become accepted as truth—a phenomenon worsened by the fact that there is sparse allergy-specific training in many medical and residency programs. It is therefore essential that case studies such as Aw’s and the larger trials that he mentioned receive the resources and funding they need to continue unravelling the mysteries of the immune system.