Ketamine, a schedule III drug, is often used recreationally for its hallucinogenic effects. Its approved purpose, however, is as an anesthetic in medical settings for animals and humans. Recently, it has also been approved by the FDA to treat major depressive disorder in patients who are resistant to other treatments.
Published in Nature, a Dec. 2020 study conducted by three Canadian universities found that the presence of a group of proteins called 4E-BPs, which are found in the brain and play a role in memory formation, enable ketamine to produce its antidepressant effect. This knowledge could be crucial in the search for alternative treatments for depression.
More than 30 per cent of patients with depression are resistant to selective serotonin reuptake inhibitors, more commonly known as SSRIs, which are the most frequently prescribed class of antidepressants. In these cases, alternative treatments for major depressive disorder are needed.
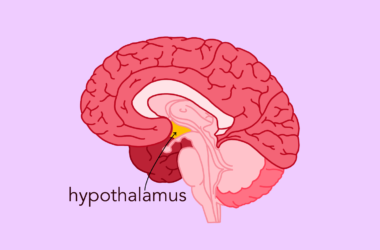
In the study, researchers removed 4E-BP proteins from specific brain cells in mice treated with ketamine and observed that protein synthesis was inhibited. Within the cells of the prefrontal cortex and hippocampus, these proteins typically regulate ketamine’s metabolites to produce an antidepressant effect. In addition, they are essential for several biological processes, including memory formation.
The elimination of 4E-BPs blocked the antidepressant effects of ketamine in both inhibitory as well as excitatory neurons. When researchers evaluated the depressive behaviour of mice with a commonly used forced swim test, they found that mice that were bred without 4E-BPs did not show improvements, suggesting the persistence of depressive behaviour. However, mice with active versions of 4E-BPs performed significantly better in these behavioural tests when treated with ketamine.
Gabriella Gobbi, a professor in the Department of Psychiatry at McGill, says that ketamine-based drugs are a last resort for patients who are resistant to common treatments.
“The first line for people suffering from depression is the SSRIs or other class of antidepressants [such as] SNRI [and] alpha-2 antagonists,” Gobbi wrote in an email to The McGill Tribune. “If the patient does not respond, there is the second line, by potentiating with antipsychotics [like] quetiapine [and] aripiprazole. Finally, the third line, in case of non-response, is ketamine or TMS.”
The use of ketamine as a treatment is somewhat controversial, mainly due to its addictive properties. However, this risk can be mitigated when supervised by health professionals. Additional clinical studies are needed to provide more information on appropriate dosages.
“In a medical setting, ketamine is used at very low doses and in a limited number of infusions […], thus the risk of addiction is minimal,” Gobbi said. “But of course, in the black market, the addiction to ketamine is an important health problem.”
Even at low doses, ketamine may not be an accessible treatment to all patients who can potentially benefit from it. According to Gobbi, the treatment must be administered under very specific conditions in specialized clinics at a hospital. Gobbi also pointed out that the price of the treatment is very high and not covered by the Régie de l’assurance maladie du Québec (RAMQ).
A personalized approach to medicine is especially important in psychiatry for several reasons. Major depression is an umbrella term that includes many subtypes of depression like bipolar, unipolar, and depression caused by medical diseases.
“This [classification] requires a very meticulous evaluation, assessment and, of course, personalized treatment, including not only antidepressants but also psychotherapy and psychoeducation,” Gobbi said.
The study’s insights into the molecular mechanisms of ketamine, such that 4E-BP proteins play a major role in its antidepressant effects, is crucial for designing new alternative depression treatments.
“Today, the studies of molecular biology, physiology, and pharmacology are helping us to better understand mental diseases and their treatment,” Gobbi said.