Just hearing the “C” word is enough to send chills down anyone’s spine—and with cancer warnings splashed across everything from cigarette packages to coffee cups, it’s difficult to avoid. In 2017, the Canadian Cancer Society amassed over $80 million in donations. According to their 2017 report, 206,200 Canadians are expected to develop cancer within their lifetime, and 80,800 will die of the disease.
Donations are often funnelled into research on high-profile cancers, like breast cancer, that boast highly successful charities. Meanwhile, ovarian cancer receives little funding despite its status as the most fatal gynecological cancer in Canada.
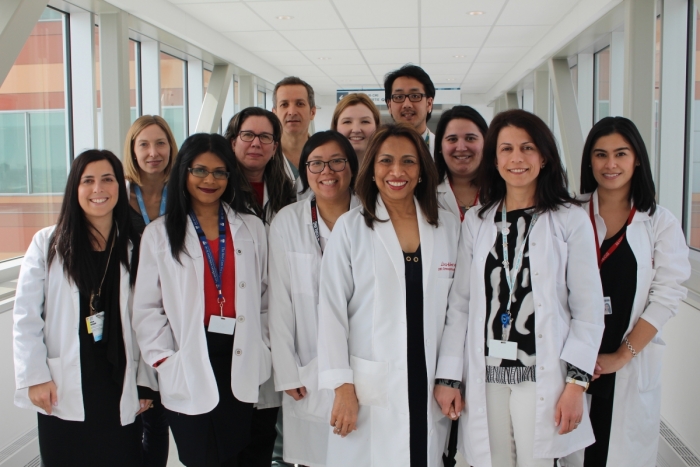
However, new hope for early detection springs from the Research Institute of McGill University Health Centre (RI-MUHC), which has overcome a critical obstacle in developing new methods of screening for ovarian and endometrial cancers in collaboration with Johns Hopkins University.
Currently, screening is not recommended for ovarian cancer due to a lack of effective methods. The difficulty in screening lies in the fact that ovarian and endometrial cancers are heterogeneous diseases, comprising of multiple subtypes that vary in fatality rates.
“In ovarian [and endometrial] cancer, the subtype that causes most of the deaths is called type two variety, [or] high-grade serous cancer,” Dr. Lucy Gilbert, director of Gynecological Oncology at the McGill University Health Centre and corresponding author of the study, told The McGill Tribune.
Unfortunately, current technologies are limited, and the type two subtype is often only detected in its third or fourth stage, by which time it’s often too late for the patient. Testing for the disease is limited to the CA 125 blood test and ultrasound imaging, neither of which can detect high-grade serous cancer in its critical early stages.
“Before [type two ovarian and endometrial cancers] cause symptoms [like] bleeding or bloating [or can be detected by imaging] they have to reach a certain volume,” Gilbert said. “At the moment, we don’t have any test that can pick it up […] before it spreads from the organ of origin [or beyond Stage 1].”
The genius behind Gilbert’s approach is targeting the earliest step in carcinogenesis: Mutations within the cell. PapSEEK, the new test described in the team’s publication in Science Translational Medicine, looks for mutations associated with these cancers by analyzing pap tests from the uterus and cervix.
“We have been looking for a test that can pick these cancers up even earlier when it’s tiny and microscopic before it causes symptoms [and] can be seen on imaging,” Gilbert said. “And the principle behind these tests [is mutations].”
Upon mutating, these cancerous cells “exfoliate,” losing their ability to adhere to one another. Even if the cancer originates in the fallopian tubes or the ovaries, exfoliated cells find their way into the uterine cavity and cervix, where Gilbert has found these flakey, mutated cells.
“By collecting cells from the cervix, and looking for these mutations that are specific to ovarian and endometrial cancer, you can identify these cancers very, very early,” Gilbert said. “[By collecting from the uterus], we were able to increase the sensitivity of the test from 33 per cent for ovarian cancer to 45 per cent, and 78 per cent to 93 per cent for endometrial cancer.”
The team’s success has drawn attention to a larger issue: The absurd lack of funding for ovarian cancer research. Between 2010 and 2014, ovarian research received only $16.9 million in funding, $64.4 million less than the funds allotted to breast cancer research. Funding, Gilbert said, continues to be disappointing.
“Women […] end up costing health care services [huge amounts] simply because of the volume of deaths and suffering, and there’s not enough funding going into it,” Gilbert said. “[PapSEEK needs] large amounts of funds [to continue its research]. We have started on a small scale but we expect to have to [continue] for another three to four years before we can get sensitivity higher and [increase] specificity.”