Human Immunodeficiency Virus (HIV) is a viral infection characterized by its ability to harm white blood cells that are crucial for the immune response. This makes HIV patients very susceptible to slightly or moderately acute diseases (that would not normally pose a serious risk for healthy individuals) by diminishing their immune system’s efficiency. If HIV progresses, it will lead to the potentially lethal stage of Acquired Immunodeficiency Syndrome. Around 1.5 million people worldwide were infected with HIV in 2021, and the virus took the lives of 650,000 people that year.
A paper published in Nature Medicine by Dr. Björn-Erik Ole Jensen from Düsseldorf University and his team this February reported that HIV was cured in a patient who had undergone a surgical transplantation of hematopoietic stem cells (HSC) – a cell type that produces blood cells. To understand the scope of Jensen’s work and its potential implications, The Tribune spoke to Anne Gatignol, a professor in McGill’s Department of Medicine and Microbiology & Immunology, who has been researching HIV for 35 years.
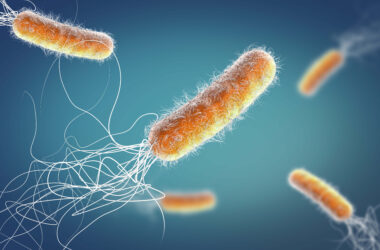
HIV is a retrovirus, meaning it uses single-stranded ribonucleic acid (RNA) to store its genetic material. Once HIV infects cells, it incorporates its RNA into the host cell genome, making it virtually impossible to cure. Nevertheless, there are currently ways to diagnose, treat, and prevent disease transmission. Unlike a cure, a treatment does not eradicate the virus from infected cells but still prevents it from exerting its damaging effects.
“Once [viral] DNA is incorporated into the host chromosome, it [becomes] part of the replication cycle. The reason why it’s so difficult to treat [HIV] is because once it is [in the genome], [it] cannot [be] remove[d] from the cell,” Gatignol said. “If you want to treat it, you have to kill the cell, but you can stop the replication cycle with drugs.”
Human immune systems mount a response against pathogens by generating antibodies—Y-shaped molecules secreted by B cells—which are essential in clearing the infection. Yet antibodies are not quite as effective in fighting HIV.
“The immune system does target HIV and cells infected with the virus [with antibodies], but the virus keeps mutating to evade the immune response. It is an ongoing battle between the virus and the new emerging immune responses,” Robert Scarborough, research associate in Dr. Gatignol’s lab, said. “Then also because [HIV] can lay dormant in cells without expressing [viral proteins], these cells are resistant to the immune system and to drugs. And that means it is there forever.”
HIV takes advantage of cell surface molecules on the surface of white blood cells known as co-receptors to enter its target cells. Two main co-receptors have been shown to be involved in HIV infection—CCR5 and CXCR4. Co-receptors are molecules that are typically found on the surface of cells and other molecules and such receptors are involved in letting the viral particles into the cell
Individuals who lack these co-receptors are naturally resistant to HIV. This gives rise to the rationale behind HSC transplantation: If you can replace the white blood cells of an HIV patient with donor cells from someone who lacks co-receptors, it could cure HIV.
Gatignol explained that HSC transplantation is traditionally used to replace the blood cells of a patient with blood cancer. In the case of Jensen’s patient, the donor’s cells had a CCR5 mutation and thus didn’t express a co-receptor necessary for the HIV to enter cells. As a result, the blood cancer treatment cured HIV as a ‘by-product.’
However, HSC transplantation may have many complications—one concern is that there is a chance the new immune cells will attack the host.
“For the HSC transplantation, risk [of death] has been estimated 10 to 12 per cent at the time of the transplantation, but 40 to 45 per cent after one year. So, globally, the risk is very high,” Gatignol said. “But the risk of HIV[-related death] is now very low, and people living with HIV now live almost complete lives.”
Thus, HSC transplantation is unlikely to become a commonplace HIV cure due to its risks but also because of small patient sample sizes in such studies, making it difficult to generalize obtained results to wider, more variable samples. Nonetheless, HSC transplantation can give us valuable clues on how to develop therapeutic treatments for HIV.
“The field that we’re working towards is to take a person’s own cells and to engineer HIV resistance in the person’s own cells—you eliminate the possibility of having the grafted cells attack the recipient’s cells—graft versus host disease—because you’re taking the person’s own cells,” Scarborough said. “That’s where we could go to [find] a cure for HIV that would be acceptable and safe for all individuals, not just those who require a transplant [due to] cancer.”