Human papillomavirus has been found in more than half of young adults in new sexual relationships, a groundbreaking Montreal study has reported.
Led by Dr. Eduardo Franco¬ – director of McGill University’s Cancer Epidemiology Unit – and a team of McGill and University of Montreal researchers, the study reported that 56 per cent of participants were infected with at least one type of HPV and 44 per cent of that group were infected with a high-risk type of the disease known to cause cervical cancer. They also found that the prevalence of HPV in one partner was a strong predictor of HPV in the other partner.
The HPV Infection and Transmission in Couples Through Heterosexual Activity, or HITCH Cohort, study used a data set of 263 women aged 18 to 24 and their male partners, all from the Montreal area. It is the first study to focus on young heterosexual couples in new relationships, the period when most transmissions of the virus occurs between partners.
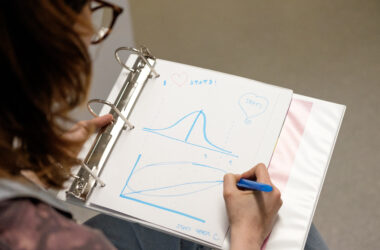
“We have really focussed on the window where transmission of the virus is most likely to occur to know how common HPV is in those partnerships and to know the potential of its transmission when you have a new partner,” said Dr. Ann Burchell, project co-ordinator and former post-doctoral fellow with Franco.
Understanding transmission between partners is what makes this study so groundbreaking. While most HPV studies focus on only one gender, HITCH looks at couples to understand and discover how easy it is for HPV to be transmitted, what factors make it easier to transmit, and what factors stop it from transmitting.
“Internationally, we are the only study of this kind,” Burchell said.
HPV is a very common group of viruses, most of which are asymptomatic and inconsequential. Generally, individuals who contract the virus will not have any manifestations, and the body will flush away the infection in 16 to 18 months. Only a few of the lower-risk strains can cause genital warts.
“You can compare it to the common cold,” Burchell said. “It’s hard to go through a whole winter in Canada without catching it.”
But as research has shown, some forms of HPV can cause cancer. High-risk types of HPV can lead to cervical cancer, which is the second most common cancer site among women after breast cancer. Other cancers, such as cancer of the penis, the vagina, the vulva, and the throat, can be caused by the virus, but these are extremely rare.
Cervical cancer isn’t particularly common, either. According to Franco, a woman who engages in sexual activity has a 0.5 per cent chance of getting cervical cancer in her lifetime.
“However, one case of cervical cancer is just the tip of the iceberg,” Franco said. “Below the tip, you have 100 pre-cancerous lesions that need to be identified by doctors. That is what needs to be discovered and prevented.”
Currently, there is no need to test directly for HPV because there are no mandated clinical guidelines to do so. An HPV test is issued only if there is an abnormal pap test. Dr. Pierre-Paul Tellier, director of the McGill Student Health Services, said that McGill can administer pap tests. However, an HPV test would be a cost to the patient. This is something that researchers on the HITCH study are trying to work on.
“We find, in our research, that testing for the virus is much more effective than testing through the pap test,” Franco said. “But this is all research in motion and the guidelines are not being rewritten yet.”
Both Franco and Burchell would like the study to promote prevention and awareness of the disease, whether through condom use, abstinence, or vaccinations. Canada has approved and is currently administering Gardisil, which protects against four strains of the virus, including two of those that are in the high-risk category. Although it is recommended for women to get the vaccination before they become sexually active, it is not discouraged for older women or even men.
“The best bang for the buck is to vaccinate at the youngest age possible, before they have sex,” Franco said. “There are diminishing gains over time as the vaccine will not flush out a virus that is already there, but acts as long-run protection.”
According to Tellier, getting the vaccination is routine and easy. The Students’ Society’s health plan pays for $300 worth of vaccinations per year, which covers almost three-quarters of the final cost.
“This is definitely something students should take advantage of,” said Tellier.