Ovarian cancer is the fifth-most diagnosed cancer among Canadian women, accounting for four per cent of all new cases. Tragically, 75 per cent of these new cases prove terminal within five years of their diagnosis. Although it is often compared to breast cancer, ovarian cancer is, in fact, more deadly, because detection usually occurs at a relatively advanced stage.
“Breast cancer patients die—not because of the cancer itself, but because of the migration of the cancer cell, while ovarian cancer patients die because it cannot be controlled,” Dr. Patricia N. Tonin, cancer researcher at the Research Institute of the McGill University Health Centre (RI-MUHC) and associate professor in McGill’s department of medicine, said of the disease.
Recognized as the most lethal gynecological cancer, ovarian cancer differs from other forms in its aggressive characteristics and the general lack of clinical and technological advancement in treatment techniques.
While 95 per cent of ovarian cancer cases can be labeled as benign, they are treated in the same way as the malignant cases—with extensive rounds of chemotherapy and cytoreductive‡ procedures.
However, a recent study conducted by the RI-MUHC—in collaboration with the Lady Davis Institute of the Jewish General Hospital and the University of Montreal Hospital Research Centre—has discovered two distinctly different genetic patterns that will not only shed light on the biological make-up of the disease, but may also revolutionize treatment plans, which currently lack customization, by focusing separately on each of these two cases.
According to Dr. Tonin, who led the study, the underlying mechanism causing ovarian cancer is the mutated form of gene TP53, which produces an abnormal, mutant protein p53. When the protein is functioning normally, it “maintains the integrity of the genome,” by detecting massive reorganizations, which is a signal of possible mistakes conducive to the advent of cancer. The protein either decides “this is such a mess; we are going to kill the cell [or] we can fix this mistake,” Dr. Tonin said.
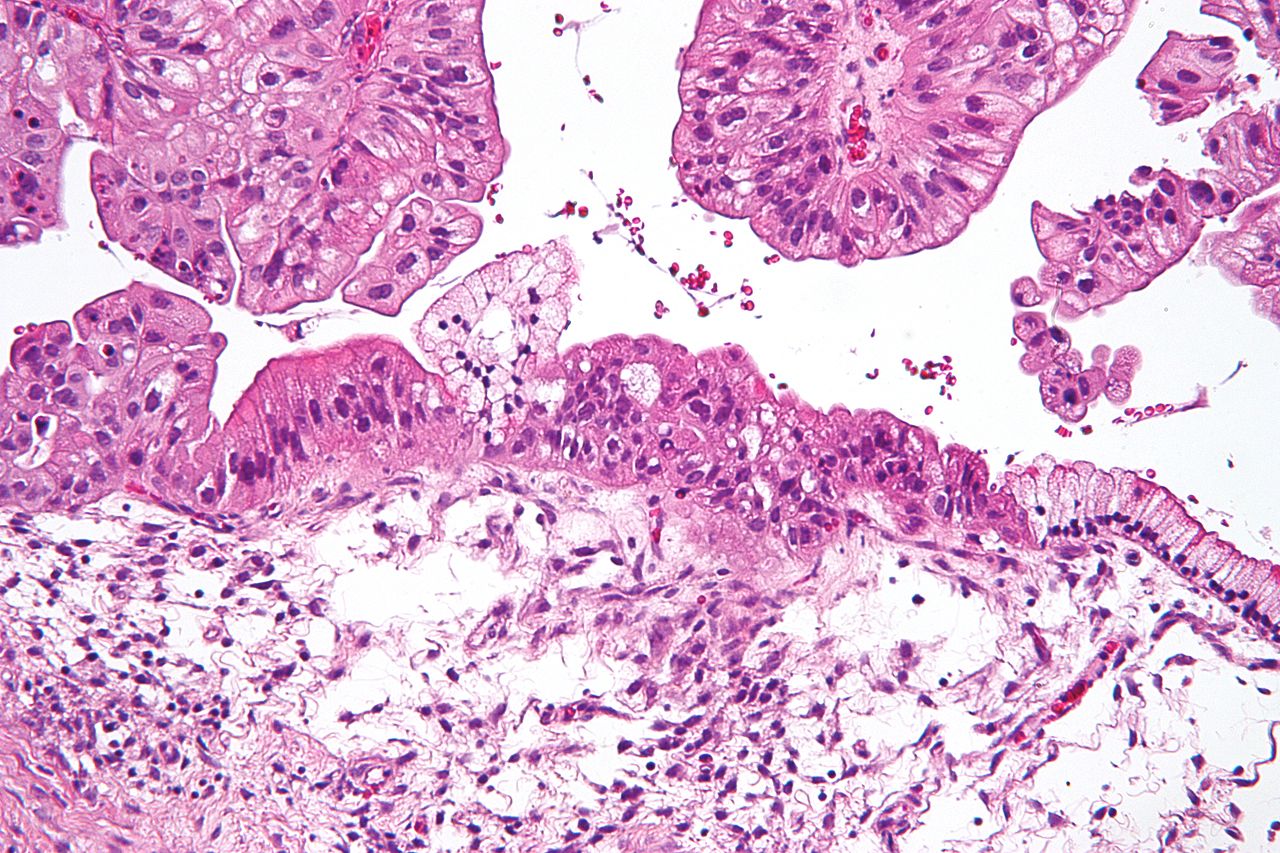
In over 90 per cent of high-grade serous ovarian carcinomas (HGSCs), a common form of ovarian cancer, the gene that has been mutated is typically responsible for sensing problems with the organization of the genome. The mutant gene instead blocks any opportunity to dispose of the troublesome cells.
The consequences of ovarian cancer vary dramatically across cases, based on the biology of the protein. A cell with mutated TP53 either may or may not produce a mutant p53 protein, and these two outcomes are directly linked to the survival rate of ovarian cancer; the former results in longer survival times and delays in cancer cell reoccurrence than the latter. This is a groundbreaking discovery because it is the first to uncover the biological difference between the two genetic patterns of ovarian cancer.
Dr. Tonin’s research paves the way for future studies into the pharmaceutical solutions to cancer. Scientists will continue working to find medications that are specifically targeted at each individual pattern, so as to reduce the invasiveness of future clinical procedures, and improve the overall outcome of treatment plans.
“Our next step,” Dr. Tonin said, “is to replicate our findings with publicly available datasets, separate the samples into two groups, and see if the patients actually survive longer, and also to generate more sophisticated data points to identify the genes involved in a more specific way.”
‡Cytoreductive: reducing the number of cells, as in surgery for a tumor.